Have you noticed your breakouts worsen after indulging in sugary desserts for a few days? Many people with acne believe sugar triggers their breakouts. However, healthcare professionals don’t often recommend reducing sugar intake as a treatment for acne due to limited evidence and the complex factors behind acne development.
- High sugar and refined carbs may trigger acne by increasing inflammation and oil production.
- Reducing high-glycemic foods can improve skin health and overall well-being.
- Individual differences mean the effect of sugar on acne can vary greatly between people.
- Dietary choices, like whole foods, can enhance skin health while reducing breakouts.
- Consulting a dermatologist is recommended for personalized acne management strategies.
Scientists continue to explore the link between sugar and acne. Although research offers mixed results, promising evidence suggests that consuming high amounts of sugar and refined carbohydrates may trigger or worsen breakouts. The effect, however, varies from person to person. Let’s dive into the reasons behind this connection, but one thing is for certain—what you eat is a critical part of your skincare routine, just like a serum or SPF.
The Science Behind Sugar and Acne
Eating too much sugar may contribute to acne by raising blood sugar and insulin levels, triggering more oil (sebum) production and increasing inflammation. High sugar intake may also lead to hormonal imbalances and the formation of advanced glycation end products (AGEs), which can damage the skin. Several studies support these associations. A study published in JAMA Dermatology found that adults with acne were more likely to consume sugary foods and drinks than those without acne. Another report from the American Academy of Dermatology suggests that high-glycemic diets (those that spike blood sugar quickly) may promote acne by increasing inflammation and sebum production. However, acne triggers vary from person to person, and more research is needed to understand how sugar affects skin health.
Should You Avoid Sugar If You Have Breakouts?
Reducing your intake of high glycemic load foods, like sugar and refined carbohydrates, can help prevent and treat acne. While the exact amount of these foods that influences acne is still unclear, cutting back can improve your overall health. You may even see noticeable improvements in your skin.
That said, the effect of sugar on acne varies from person to person, and there’s no one-size-fits-all solution. For a comprehensive approach to managing acne, it’s best to work closely with a dermatologist. Reducing high-sugar and high-glycemic foods, while focusing on a balanced diet rich in whole foods like fruits, vegetables, nuts, and seeds, may also help improve acne symptoms.
Does Glycemic Index (GI) Play A Role in Sugar Causing Acne?
Glycemic index (GI) is a scale that ranks carbohydrates based on how quickly they raise blood sugar levels. Some studies suggest that high-glycemic foods, which cause a rapid spike in blood sugar, may contribute to the development or worsening of acne.
The theory behind this connection is based on the hormonal response triggered by high-glycemic foods. When you eat these foods, they can cause a rise in insulin and insulin-like growth factor 1 (IGF-1) levels. Elevated levels of these hormones may increase sebum production, skin cell growth, and inflammation, all of which contribute to acne development.
It’s important to note that research on this topic is mixed. Not all studies have found a clear link between glycemic index and acne. Other factors, like genetics, overall diet, and individual differences, can also influence acne. If you’re concerned about how glycemic index might affect your acne, try incorporating more low-glycemic foods into your diet, as they cause slower increases in blood sugar levels.
Other Dietary Triggers for Acne
Certain foods may contribute to acne by affecting hormones, inflammation, and oil production. While research is ongoing, these are some common dietary triggers:
- Dairy products: Milk and other dairy products contain natural hormones that may increase oil production and worsen acne in some people.
- High-glycemic foods: Foods like white bread, pastries, and sugary cereal cause blood sugar spikes, leading to inflammation and excess sebum production.
- Processed and fried foods: These foods often contain saturated fats and additives that may promote inflammation, a key factor in acne development.
- Whey protein supplements: Often found in protein powders, whey protein may increase insulin and IGF-1 levels, stimulating oil production and acne.
- Alcohol: Some alcoholic beverages, especially sugary cocktails, may contribute to inflammation and dehydration, affecting skin health.
Since dietary effects vary from person to person, it’s important to track your triggers, as what causes breakouts in one person may not affect another. A Registered Dietitian can help you narrow down your triggers and determine which interventions may work best for you.
High-GL Foods To Avoid If You Have Acne
Most of the better-quality studies on sugar and acne examined the effects of eating a high glycemic index diet on acne development and severity. However, the glycemic index (GI) isn’t used frequently because it doesn’t consider serving sizes or the nutritional benefits of different carbohydrates. Conversely, Glycemic Load (GL) measures how certain foods impact blood sugar based on standard serving sizes of specific foods. Foods that score high on the GI also may significantly increase your blood sugar compared to low-GL foods.
Examples of High-GL Foods
- Products made with white flour (breads, bagels, pastas, and desserts): These foods are often processed and refined resulting in a loss of fiber and nutrients. They are quickly broken down into glucose, causing a rapid rise in blood sugar levels.
- Soda: Regular soda contains high amounts of added sugars which contributes to its high glycemic load.
- Juice: Many fruit juices have a high concentration of natural sugars without the fiber found in whole fruits. This lack of fiber allows for quick absorption of the sugars, resulting in a high glycemic load.
- Desserts and candy: These items are typically high in added sugars, which can quickly raise blood sugar levels and contribute to a high glycemic load.
- Sugar: Pure sugar, whether added to foods or consumed on its own, has a high glycemic load as it is rapidly absorbed by the body.
- Sweetened cereals: Many breakfast cereals contain added sugars. These sugars are rapidly digested and absorbed, leading to a high glycemic load.
- White rice: White rice has been processed and stripped of its bran and germ, resulting in a lower fiber content and faster digestion. This causes a quick release of glucose into the bloodstream and a higher glycemic load compared to whole grains.
- Dried fruits: While dried fruits can be nutritious and provide essential vitamins and minerals, they can also have a high glycemic load due to their concentrated sugar content.
Some studies suggest that a high-glycemic load (GL) diet may increase the development and severity of acne. A systematic review published in JAAD International found that a high glycemic index, increased glycemic load, and higher carbohydrate intake had a modest but significant acne-promoting effect. Another study found that participants on a low-GL diet had lower levels of sebum production. Excess sebum production is a known risk factor for acne development.
Eat These Foods For Better Skin
Food is a critical part of your skincare routine! Nutrition greatly impacts all parts of the body, including the skin. Changes in skin texture, color, dryness, temperature, and overall appearance are among the first signs of nutrient deficiency and other health concerns.
A balanced eating routine with a variety of fruits, vegetables, lean protein, healthy fats, and complex carbohydrates provides nutrients to support the skin’s growth and recovery. Supporting this process of growth and recovery is key to a healthy, nourished skin. It’s also important to avoid eating patterns that may negatively affect this process and introduce ingredients that can cause harm to the skin.
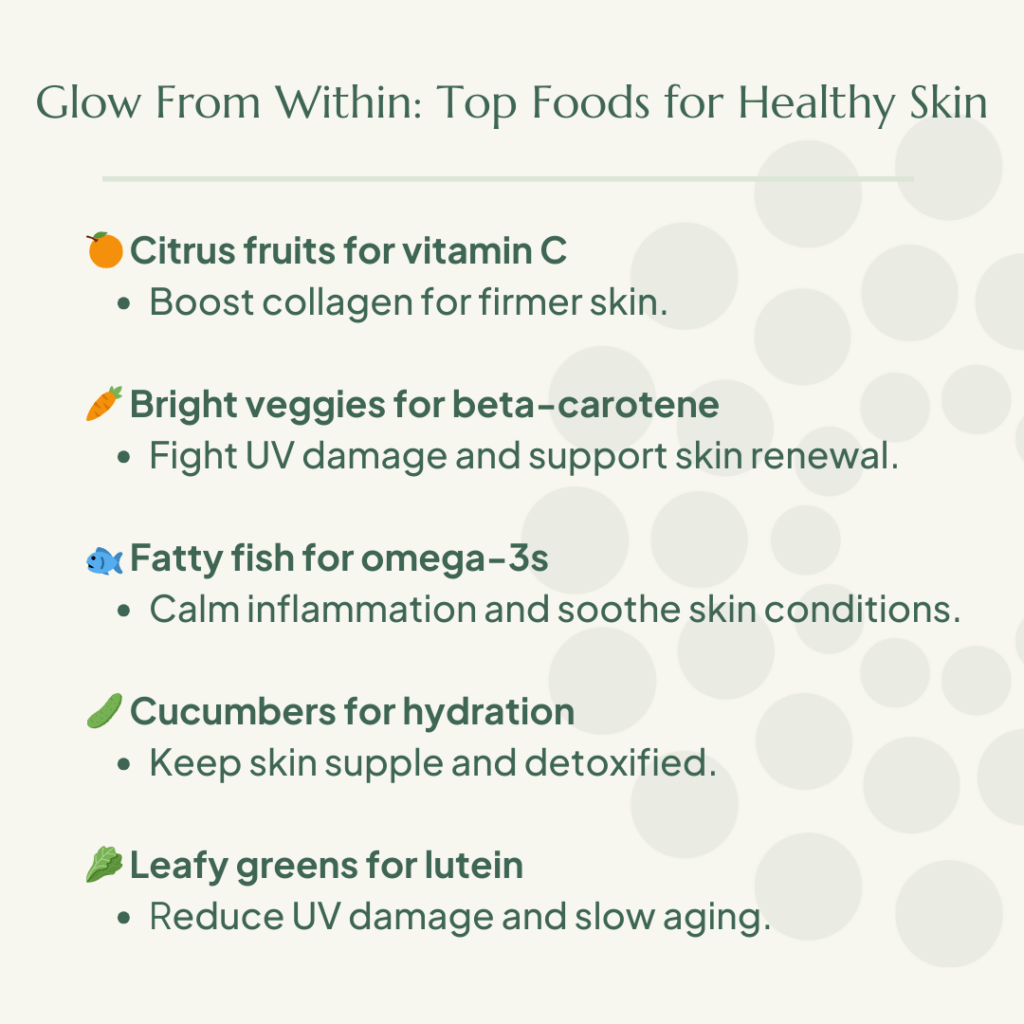
Best Foods for Skin Health
- Citrus fruits, such as oranges and lemons, are excellent sources of vitamin C, which is crucial for collagen production. Collagen is a vital protein that provides structure to the skin, bones, muscles, and connective tissues. It promotes cell renewal, aids in cell repair, and helps prevent sagging skin, a common sign of aging.
- Bright orange and yellow fruits and vegetables contain beta-carotene, which is converted into vitamin A in the body. Vitamin A acts as a potent antioxidant, protecting skin cells from UV damage and premature aging. It also supports cell growth and stimulates collagen production, contributing to healthier skin.
- Fatty fish like salmon, mackerel, and sardines are rich in omega-3 fatty acids, specifically DHA and EPA. These fatty acids have anti-inflammatory properties, which can help reduce inflammation in the body. Inflammation can damage skin cells and contribute to skin conditions like acne, rosacea, and psoriasis.
- Cucumbers, with their high water content, can contribute to your daily hydration needs. Proper hydration is essential for skin health as it keeps the skin hydrated, supports elasticity, and aids in the removal of waste and toxins from the body, which can harm the skin.
- Leafy green vegetables, such as spinach and kale, contain lutein, an antioxidant that helps reduce oxidative and UV damage to skin cells. By reducing premature aging caused by environmental factors, lutein contributes to healthier and more youthful-looking skin.
Incorporating these nutrient-rich foods into your diet can provide essential vitamins, antioxidants, and omega-3 fatty acids. These nutrients support skin health and collagen production. They also help protect against various skin issues and signs of aging.
Practical Tips for Reducing Sugar Intake
Making small, sustainable changes to your diet can help reduce potential acne triggers and support overall skin health. Try these easy adjustments:
- Swap sugary snacks for fresh fruits or nuts: This helps to reduce inflammation and stabilize blood sugar while providing skin-friendly nutrients.
- Choose whole grains over refined carbs: Opt for whole wheat or multigrain bread, oats, brown rice or quinoa instead of their refined counterparts such as white bread and white pasta
- Swap dairy milk for a plant-based alternative if dairy triggers breakouts.
- Use baking or air-frying cooking methods to reduce excess oil and saturated fats.
- Read food labels to spot hidden sugars in processed foods, such as in packaged foods like yogurt, granola bars, and salad dressings.
- Limit sugary drinks like soda and flavored lattes, opting for water or unsweetened beverages like herbal tea, infused water, or unsweetened alternatives to keep your skin hydrated and reduce sugar intake
- Snack on trail mix with nuts and seeds to provide skin-loving nutrients such as zinc and omega-3s.
- Swap high-sugar yogurt for unsweetened Greek yogurt with berries
Start small! Making gradual changes makes them more sustainable. Just one change can have a big impact not only on your skin but on your overall health.
FAQs About Sugar and Acne
Can sugar cause breakouts in adults?
Yes, sugar can contribute to breakouts in adults, primarily through its effects on hormonal balance and inflammation. When you consume high-sugar foods, your blood sugar spikes, causing a surge in insulin and insulin-like growing factor (IGF-1). These hormones can increase sebum (oil) production and trigger inflammation (two key factors in acne development). Additionally, sugar can disrupt other hormones, such as androgens, which may further aggravate breakouts, particularly in individuals with hormonal acne, PCOS, or insulin resistance.
How quickly does sugar impact acne?
The timeline varies from person to person. Some people may notice breakouts within a few days after consuming excess sugar, while for others, the effects are more gradual. Regular excess sugar intake over time is more likely to have a cumulative effect, contributing to persistent acne due to ongoing inflammation and hormonal fluctuations. Occasional sugar consumption may not trigger breakouts in everyone, but frequent spikes in blood sugar can set the stage for long-term skin issues.
Does cutting out sugar improve acne?
Reducing sugar can help improve acne for some people, but it’s not a guaranteed solution. Since acne is influenced by multiple factors (including hormones, genetics, stress, and skincare habits), cutting sugar alone may not completely clear the skin. However, many individuals notice reduced inflammation, fewer breakouts, and overall improved skin health when they follow a balanced, nutrient-dense diet with low sugar intake.
Are natural sugars like fruit also linked to breakouts?
Fruits contain natural sugars, but they are also rich in fiber, vitamins, antioxidants, and water, which help slow down sugar absorption and reduce insulin spikes. Unlike added sugars, most low-glycemic fruits such as berries, apples, and oranges are not strongly linked to acne. However, high-glycemic fruits like watermelon and ripe bananas could contribute to breakouts in some people when consumed in excess. The key is to focus on a balanced diet rather than avoiding all sugars entirely.
The Bottom Line
Achieving optimal skin health and managing acne involves several factors. For example, genetics play a role in your susceptibility to acne. A balanced diet, tailored skincare, hormonal balance, and managing stress all contribute to healthy skin. Getting enough sleep and minimizing exposure to irritants are also important. Regular exercise further boosts skin health. Seeing a dermatologist offers personalized advice and treatment options tailored to your specific skincare needs. If you’re seeking ways to improve your skin’s health, get matched with a Culina Health dietitian to support your health goals from the inside out.





