How a Registered Dietitian Can Help People With Diabetes
If you’re living with diabetes or prediabetes, you’re not alone. About 38 million people in the U.S. have diabetes, and almost 98 million have prediabetes.
- Registered dietitian nutritionists (RDNs) provide personalized nutrition plans based on health history and lifestyle for diabetes management.
- Physical activity is crucial for improving insulin sensitivity and lowering blood sugar levels while managing diabetes.
- Setting small, achievable goals aids in creating sustainable lifestyle changes to effectively manage diabetes.
- Dietitians help address food fears, promoting a balanced approach to nutrition that respects individual preferences and cultural backgrounds.
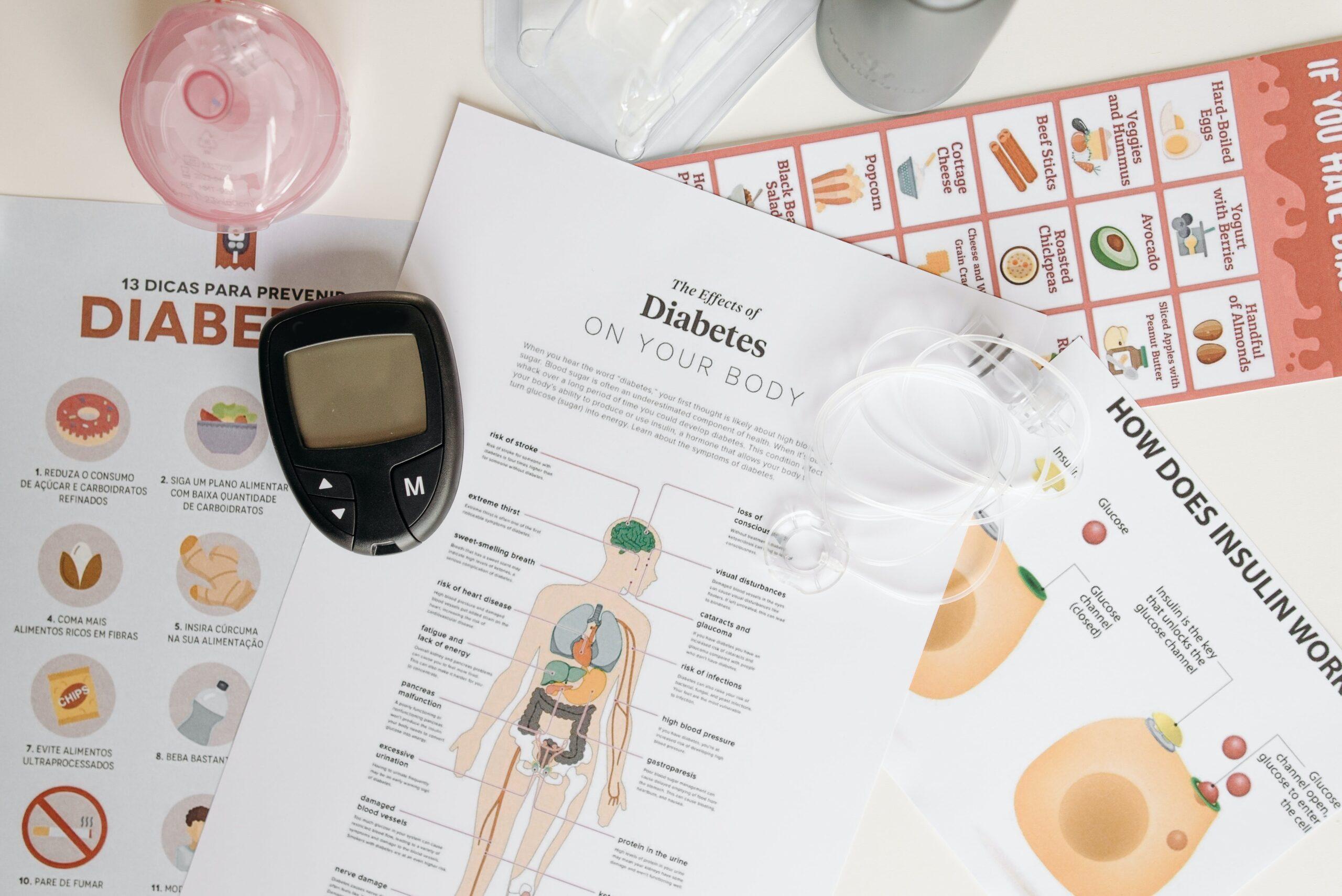
Diabetes is a chronic disease that affects how your body maintains your blood sugar, or blood glucose levels. Glucose levels can rise in response to food intake, or other physiological processes, such as stress or illness. When these levels rise, the pancreas releases a hormone called insulin. Insulin tells your body that extra glucose is available, and helps move the sugar out of your bloodstream and into your cells for energy or storage.
If you have diabetes, your body either doesn’t make insulin or doesn’t respond to insulin, causing sugar to accumulate in the blood. For most patients, nutrition can play a significant role in diabetes management or prevention. A registered dietitian nutritionist (RDN) can help you identify and enact lifestyle changes that help keep your glucose in a healthy range.
What Does a Dietitian Specializing in Diabetes Do?
A dietitian specializing in diabetes provide medical nutrition therapy to patients who are living with diabetes or prediabetes. The dietitian will consider their patient’s health history, dietary preferences, medication, lifestyle, and goals when developing a personalized nutrition care plan. Diabetes care is definitely NOT one size fits all!
A dietitian can also help patients manage or reduce risk of diabetes-related complications, such as digestive, heart, and kidney diseases. Additionally, the dietitian can collaborate with primary care physicians and specialists to integrate nutrition into their patients’ diabetes care plans.
Types of Diabetes
Type 1, type 2, and prediabetes are the most common types of diabetes that I see in my practice. I also support patients with gestational diabetes, a temporary rise in blood sugar during pregnancy due to hormones.
Diabetes may present with various symptoms depending on your average glucose levels and whether you have developed any diabetes-related complications. Many people will experience high blood sugar symptoms in the days or weeks leading up to their diagnosis. These include excessive thirst, excessive hunger, frequent urination, fatigue, and blurry vision.
If your glucose remains above target for a prolonged amount of time, you may experience symptoms associated with nerve and blood vessel damage, such as tingling, pain and numbness of the lower extremities, or vision loss.
Type 1 Diabetes
Type 1 diabetes (T1D) is an autoimmune condition in which the body does not produce any insulin due to destruction of beta cells in the pancreas. Though previously associated with diagnosis during childhood, this condition can present at any age. Type 1 diabetes is currently thought to be caused by a combination of genetics and environmental triggers.
If you were recently diagnosed with type 1 diabetes, a registered dietitian (RD) can help you understand how different foods impact your blood sugar. We can also help you learn carbohydrate counting if that is part of your care plan. If you’ve been living with T1D for some time, a registered dietitian can partner with you to evaluate trends in your glucose, food, and exercise logs to identify opportunities for modification if necessary.
Type 2 Diabetes
When you have type 2 diabetes (T2D), your cells become resistant to insulin. This means that sugar has trouble passing into cells and stays in your blood. Your pancreas may be able to make extra insulin temporarily, helping to keep blood sugar levels closer to target range. But over time, the pancreas may not be able to keep up, causing blood sugar levels to rise further. T2D is also greatly influenced by genetic predisposition and environmental exposures. However, diet and lifestyle factors can play a more significant role in disease progression for some.
Prediabetes
Healthcare providers often diagnose individuals with prediabetes before identifying type 2 diabetes. Patients with prediabetes are usually experiencing insulin resistance. This causes glucose levels to rise slightly, but they are still producing enough insulin to keep blood sugar below the diagnostic threshold for diabetes. With a few lifestyle changes, many patients can bring their average blood sugar levels down and prevent progression to T2D.
What would these lifestyle changes look like? Current evidence shows that there isn’t one ideal diet for the prevention of diabetes. Patients can adopt various healthy eating patterns, from Mediterranean to plant-based (spoiler alert: low carb is one option, but it’s not the only option). Regular physical activity is also a key part of diabetes prevention. A registered dietitian can help patients with prediabetes identify and implement the lifestyle modifications that would work best for them.
5 Ways a Registered Dietitian Can Help People With Diabetes
A registered dietitian nutritionist can be a valuable part of the healthcare team for people with diabetes. We can offer strategies to help you successfully integrate carbohydrates, leverage physical activity, optimize meal and snack planning, decide how weight will factor into your care plan, and set goals for lasting lifestyle modification.
Integrating carbohydrates
Carbohydrates contribute most significantly to blood sugar changes. While they’re are not off limits for people with diabetes, it’s important to understand how carbohydrate-rich foods impact blood sugar. Carbohydrate-rich foods include fruits, starchy vegetables, grains, grain products, legumes, milk, yogurt, concentrated sweets (like candy, ice cream, and baked goods), and sweeteners (like sugar, honey, and maple syrup). Our gut breaks the carbohydrates down into glucose, which our bodies absorb and use for energy.
You’ll need to consider three factors when consuming carbs:
- What kind? Choosing fiber-rich fruits, vegetables, legumes, and whole grains is a great way to enjoy carbohydrates while keeping your glucose at goal. This is because fiber slows the digestion of carbohydrates into sugar, resulting in a more moderate rise in blood glucose after eating. High-fiber foods include: barley, whole grain bread or pasta, oatmeal, pumpkin, yams, apples, pears, berries, oranges, beans, and lentils — just to name a few.
- How much? A moderate portion of carbohydrates is easier for your body to handle if you have diabetes, versus a larger amount. A portion about the size of your fist is right for most people. You can eat carbohydrates multiple times per day; it’s the amount per sitting that will impact your glucose levels the most.
- What else is on the plate? I always suggest pairing carbohydrate-rich options with proteins, healthy fats, and non-starchy vegetables to further slow down the digestion of carbs. Use this approach for meals and snacks to promote steady blood sugar and satiety (fancy clinical word for “fullness and satisfaction”). My favorite combinations are whole grain crackers with avocado and bagel spice, a pear with almond butter, or apple slices with cheddar cheese.
A registered dietitian can provide specific advice on carbohydrate intake based on your height, weight, activity level, age, food preferences, and other medical conditions.
Leveraging physical activity
Regular physical activity is beneficial for managing and preventing diabetes. It increases the body’s insulin sensitivity and lowers blood sugar. It doesn’t matter what type of exercise — from walking or jogging to dancing or swimming — any consistent exercise is excellent. If you don’t exercise regularly, start with 20 minutes every one to two days, gradually building up to 30 minutes, five days per week. Try a mix of aerobic exercise and strength training!
Meal and snacking timing
Meal and snack timing can be an important part of your diabetes care plan depending on what medications you take. Some medications may cause hypoglycemia, or low blood sugar, if you go for many hours without eating.
Regular meals and snacks can also prevent excessive hunger, which makes mindful food choices difficult. When your internal gas tank is almost empty, your body will ask for plenty to eat, and fast! Making up for a skipped breakfast by eating more at lunch can pose a problem for people with diabetes, since a larger serving of carbohydrate-rich foods is more likely to cause your glucose to rise above target.
A registered dietitian knowledgeable in diabetes care can help you determine whether your medication regimen necessitates eating meals and snacks on a regular schedule. We can also help you optimize your daily routine in a way that is realistic and incorporates your preferences.
Weighing the options on weight management
Most guidelines recommend weight loss as part of a diabetes management or prevention care plan for people at higher weights. However, there is growing evidence to support a weight neutral approach to diabetes care. This means you can focus on healthy behaviors rather than the scale and still see results.
Whichever approach feels best for you, a registered dietitian can support you. We follow science-backed protocols when creating nutrition plans. This ensures that we avoid fad diets and unsustainable weight loss plans, which can lead to weight cycling and frustration. Registered dietitians can also help you set behavioral goals to increase physical activity, move toward a healthy eating pattern, and tune into hunger and fullness cues to guide portion size.
Goal setting
Goal setting is where the rubber meets the road. Setting small, achievable goals each week is the best way to build toward larger, long-term goals. Registered dietitians can help you identify the goals that will set you on the right path, support you in developing strategies for success, and help you troubleshoot obstacles along the way.
For example, let’s say you are working towards adding high-fiber carbohydrates at breakfast six days per week. Your starting goal may be to incorporate a high-fiber carbohydrate at breakfast twice a week. You and your RD will identify strategies to make it happen, whether it’s putting new foods on your grocery list or prepping the night before. Then after you get comfortable with it twice a week, your next goal might be three times a week — and so on, until you’re crushing it six times a week!
Benefits of Working With a Registered Dietitian Nutritionist for Diabetes
One of the top benefits of working with a registered dietitian nutritionist is that we love food — and we want you to love it too! RDNs understand food’s nutritional composition, and how to optimize a meal’s nutritional value using specific food combinations and preparation methods. As a dietitian specializing in diabetes care, I help my patients enjoy their favorite foods and keep their blood sugar levels in range.
Some people with diabetes also struggle with food fears, especially if they’ve been told to avoid certain foods or have had a bad experience when trying to incorporate specific foods. If you’re facing this very real challenge, a dietitian can help you explore food avoidance or restriction tendencies, understand the pros and cons of addressing these habits, and implement a plan to add variety to your diet when you are ready in a way that feels safe to you.
Diabetes, Dietitians, and BIPOC Communities
Diabetes disproportionately impacts communities of color in the U.S. Hispanic people are over 50% more likely to receive a diabetes diagnosis, with similar outcomes for African Americans (60%) and Asian Americans (40%). Contributing factors include genetics, chronic stress, built environment, access to culturally appropriate nutrient dense food, and equitable access to healthcare, among others.
Thankfully, equity and inclusion conversations in healthcare are shifting to address the systemic issues contributing to increased diabetes risk in BIPOC communities. Diabetes prevention and management support can reduce the burden of comorbidities, like renal and cardiovascular illnesses, that occur due to chronic blood sugar elevation.
As a diabetes specialist involved in direct patient care, my role is to ensure these communities have access to culturally affirming nutrition counseling and education. I invest time in getting to know my patients, learning about their lived experience, cultural foods, and health beliefs to create a realistic and authentic plan together.
What is a CDCES?
CDCES stands for “certified diabetes care and education specialist.” It’s a credential that registered dietitian nutritionists, nurses, and other healthcare practitioners can earn. Adding a certified diabetes educator to your treatment team has many proven benefits. We help patients with diabetes navigate everything from medication and glucose monitoring devices to mental health and stress management.
As a CDCES, I provide education and counseling related to all seven diabetes self-care behaviors: healthy eating, being active, taking medication, monitoring, healthy coping, problem solving, and reducing risk of acute complications (i.e. low blood sugar) and chronic complications (i.e. heart disease).
Diabetes Resources
Registered dietitians and certified diabetes care and education specialists provide resources to people with diabetes, caregivers, and family members. The American Diabetes Association, Association of Diabetes Care and Education Specialists, Beyond Type 1, and diaTribe, also provide information online. If you prefer additional support in person, your local hospital or community medical center may offer education and support programs.
How to Choose a Dietitian for Diabetes Care
When choosing a dietitian for diabetes management, it’s important to consider these factors:
- Find a registered dietitian. RDs must complete extensive clinical training to earn their certifications, which sets us apart from many other nutrition professionals.
- Check with insurance: Unlike nutritionists, most registered dietitians accept insurance. Contact your insurance provider to find out if they cover registered dietitian visits for diabetes management.
- Choose the right person: Diabetes is a complex condition that impacts many aspects of your daily life. Choosing a registered dietitian who will take time to understand your preferences and priorities is a key step toward a sustainable, successful diabetes care plan.
Schedule a consultation with a Culina Health RD to learn how we can help you manage or reduce your diabetes risk.
Any general advice posted on our blog, website, or application is intended for reference and educational purposes only and is not intended to replace or substitute for any professional medical advice, diagnosis, treatment, or other professional advice. If you have specific concerns or a situation arises in which you require medical advice, you should consult with an appropriately qualified and licensed medical services provider.





