Whether or not you struggle with how your body responds to certain foods, you may know someone who is, for example, lactose intolerant, sensitive to gluten, or has a nut allergy. But not all of these things are created equal! It’s important to understand and break down food allergies, food sensitivities, and food intolerances. So we tapped Rakhi Roy Chowdhury, MS, RDN to help us understand these topics, and offer support to those who are experiencing issues with certain foods. Read on to learn more!
About Rakhi Roy Chowdhury, MS, RDN
What was your journey to becoming an RD?
I like to say I didn’t choose this career, but that instead it chose me. I struggled with food allergies growing up, but had no clue where to turn to for support. Instead, I just did my best to live with these uncomfortable symptoms, including asthma that even led my family to move to a different state, from New York to Florida. Finally, when I was 23 years old, I visited an RD to learn more about my food allergies and what I could do about them. That encounter not only had a major impact on my health—it also completely reshaped the trajectory of my career.
How did you come to specialize in the area of food allergies?
My lived experience is what ultimately led me to take a special interest in food allergies and intolerances, and related conditions such as IBS and gut health. I saw the confusion around these conditions, and the way so many patients were left feeling unheard, like I was. I knew I could fill in that gap and provide clarity surrounding their symptoms, as well as become empowered with knowledge around what foods might make them feel a certain way, and tailor their diet toward balance and overall health and wellness.
Food allergies, food intolerances, and food sensitivities—are they different?
This is a huge misconception—because most people think that any sort of reaction is an allergy, but in reality, they are quite different, and result in different reactions of differing severities.
Food allergies
Allergies typically involve the immune system and are confirmed with the help of an allergist. The most common food allergy symptoms are hives, swelling, and anaphylaxis (a severe, life-threatening allergic reaction).
Allergies fall on a spectrum and don’t always result in anaphylaxis or a severe allergic reaction, however. For example, those with milk and egg allergies don’t always need to completely eliminate these foods if they are tolerated in a cooked or baked form. Those with oral allergy syndrome, also known as Pollen Food Allergy Syndrome, allergic to fruits and vegetables may also find they can tolerate these foods if cooked or preserved in citric acid—since heat and acids denature the proteins. Everyone has a different level of tolerance. Working with an allergist and a food allergy dietitian can help you determine this through an oral food challenge.
Food intolerances and food sensitivities
Food intolerances or sensitivities can be confirmed with a dietitian through an elimination diet followed by reintroduction. Common symptoms of food sensitivities include brain fog, joint pain, and fatigue, whereas the most frequent markers of an intolerance are GI related digestive health issues, such as bloating, diarrhea, or constipation.
Hot tip: Don’t go on a gluten-free diet before ruling out celiac disease, which is confirmed with a gastroenterologist. Doing so can significantly affect the accuracy of celiac disease test results, potentially leading to a false negative diagnosis. It’s crucial to continue consuming gluten until confirmation through celiac serology and biopsy.
If gluten has already been eliminated, then I often recommend patients undergo a “gluten challenge,” which would involve consuming 1-2 slices of bread (or equivalent amount), for at least 2 to 8 weeks prior to undergoing biopsy.
What are the most common trigger foods for allergies, intolerances, or sensitivities, and why?
The most common allergies I see are:
- Nut allergy
- Shellfish allergy
- Dairy allergy
Sensitivities I most often see are:
- Gluten sensitivity
- Dairy sensitivity
The most common intolerances I see are:
- Lactose intolerance
- Fructans (a type of sugar and fiber found in many fruits, vegetables, and grains) intolerance
These are most often caused by genetics, immune dysfunction, acute gastroenteritis, food poisoning, or low digestive enzyme activity.
What is the role of gut health in food allergies, sensitivities, and intolerances?
Between 60-80% of our immune cells reside in our gut, and there’s some research to show that intestinal permeability and gut dysbiosis (a.k.a. an imbalance of good and bad bacteria) could play a role in development of food allergies and intolerances, however much more research still needs to be done on how this can be applied in their management. However, it’s clear that digestive health plays a role in our ability to tolerate different foods.
The “dual allergen exposure hypothesis” offers one possible explanation of how allergies develop. It suggests that exposure to food allergens through damaged skin (like eczema) or via airway inhalation can lead to sensitivity and allergies, while oral exposure through the gut to the same allergen usually promotes tolerance, potentially explaining why early introduction around 4 to 6 months old of potential allergens in infants can help prevent food allergies. When exposure doesn’t occur, the likelihood of developing allergies during childhood increases.
Among adults, food allergies have sometimes been observed after prolonged avoidance of certain foods. Reintroduction of these foods can lead to reactions, likely due to sensitization via the skin or lungs. Additionally, medications affecting the gut, such as acid suppressors, have been proposed to elevate the risk of developing food reactions.
Working with Patients on Food Allergies, Food Sensitivities, and Food Intolerances
How do you approach working with patients on a suspected food allergy, food sensitivity, or food intolerance?
I always begin with a detailed history, digging into their symptoms, triggers, and lifestyle. I’ll ask patients to keep a food log as well as a symptom log, to understand the correlation between what they are eating and the symptoms that are coming up. Then, I work to investigate how severe the food intolerance symptoms are, based on their timing, when they arise, and how severe their effects are. I then make a clinical decision on whether a patient needs a referral to a specialized food allergist if they don’t already have established care.
As an RD, my work closely intersects with that of a food allergist—I help people develop a plan for eating and enjoying specific food in a way that manages symptoms, without leading them to feel too restricted. It can be hard to eliminate food triggers, especially if it’s something you enjoy. For example, if you need to eliminate dairy, that’s a major part of your diet that’s going to change. A registered dietitian can help you come up with solutions to this major change and find delicious and nutritious substitutes to add into your diet instead.
What are the most common questions you hear from patients about food allergies or intolerances?
The most common one is, “Can I ever eat this again?” Well, it depends. Some intolerances or sensitivities don’t result in severe symptoms, and for some people they can improve over time. Some allergies, however, require lifelong avoidance.
Another question I get often is whether or not someone needs an allergy test. Not always. Allergy tests can provide clues but are not 100% accurate. In fact, skin-prick tests are only about 50-60% accurate, and food intolerance or sensitivity tests that look at IgG antibodies are typically not super accurate nor are validated tests.
So, you may be wondering, how do we diagnose and treat food allergies and intolerances? In my experience, analyzing clinical history, observation through elimination diets with proper reintroduction challenges, and symptom tracking often reveal the clearest answers.
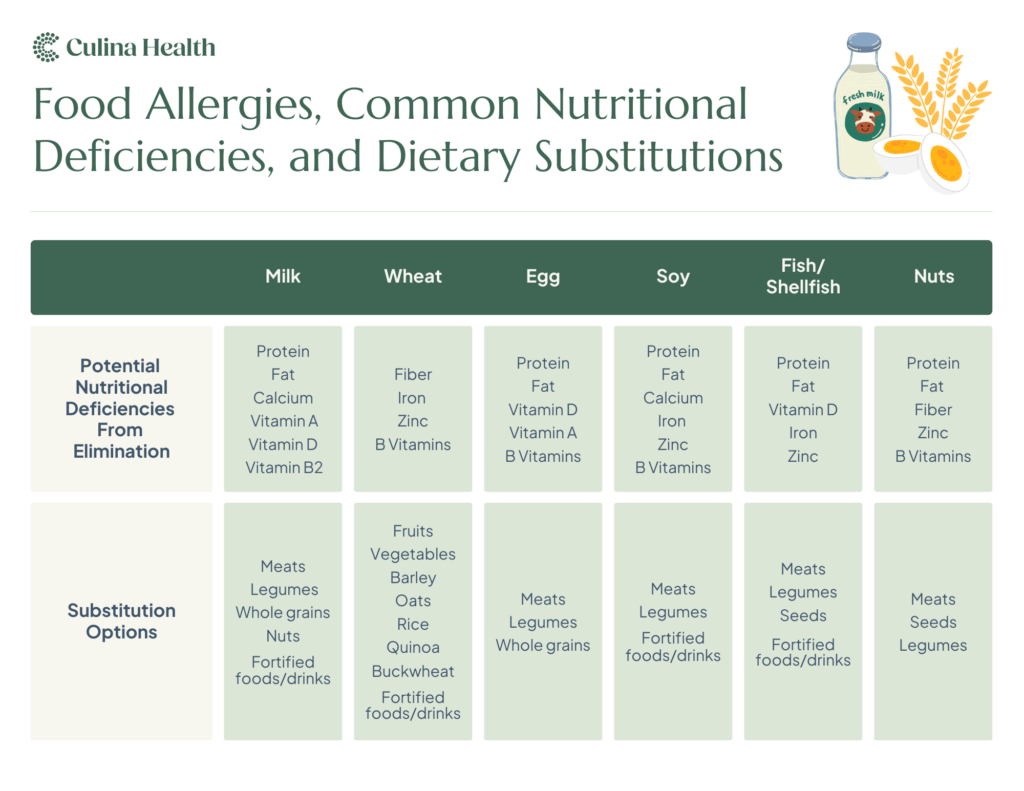
Nutrient deficiencies resulting from food allergies
One concern when a patient does need to eliminate or significantly reduce a certain food group or particular food from their diet is how they will “make up for” the nutrients they are missing out on. For example, those who have to eliminate dairy products might be at risk for deficiencies in protein, calcium, vitamin d, and more. To substitute, we might think of meat, nuts, legumes, and whole grains to add in.
What are some food allergy success stories you have from working with patients?
One patient with bloating and brain fog thought they were allergic to everything. After ruling out allergies and celiac disease, we identified a lactose intolerance and gluten intolerance. Introducing lactose-free and gluten-free options into their diet changed their energy levels and mental clarity in weeks. It also allowed them to broaden their diet by understanding their tolerance levels to certain foods and reduce the anxiety they were experiencing around food.
Another frequent success story I see is with patients who have egg allergies. Although they might not be able to tolerate raw egg (for example, sunny-side-up eggs or mayonnaise), by introducing them gradually in baked goods through a “baked egg challenge,” they’re often able to tolerate cooked eggs, such as in muffins.
Get support for food allergies from a registered dietitian
Are you dealing with symptoms you want to investigate, looking to support your immune system, digestive system, or need help reconfiguring your diet after an allergy diagnosis? Get support for this, and more, from a Culina Health dietitian. We accept most major insurance plans, so you could pay as little as $0 out of pocket per session. Get matched with a registered dietitian today.





