Keeping your blood sugar balanced is critical to so many aspects of our health, from maintaining energy levels and brain function to reducing our risk of many chronic diseases such as diabetes. And the good news? There’s so much we can do to maintain optimal blood sugar balance. To break down the ins and outs behind the science, as well as tips and strategies for controlling blood sugar, Culina Health RD Paige Heiden, MS, RDN hosted a community webinar. You can watch it here, or read below for the top takeaways!
The Science Behind Prediabetes
If you have prediabetes, it means that your body is starting to have trouble keeping the right amount of glucose (aka sugar) in your blood. But how does the sugar get there? Well, when we eat carbs, our body breaks them down into glucose, which travels from the intestines into the blood, and then heads to our cells. Cells either use glucose for energy, or they will store it to use later in the liver or muscles.
Think of your body like a house, and it has a thermostat which automatically adjusts to keep your glucose levels steady throughout the day. That thermostat, along with insulin, is what controls your blood sugar. While everyone’s blood sugar rises after they eat, even if they don’t have prediabetes, the blood sugar levels of someone with prediabetes or diabetes likely will increase at a higher, more rapid rate than that of someone without prediabetes, and have more difficulty getting back to baseline.
Let’s Talk About Insulin
Insulin is a hormone made in your pancreas that’s released into the blood when blood sugar rises above baseline. Insulin helps move glucose out of your body and into your cells, acting as a gatekeeper. Without it, glucose cannot enter cells.
For most people with prediabetes, your cells have become resistant to insulin. Insulin is knocking at the door of each cell, but no one is home. As a result, sugar has trouble passing into cells and more stays in your blood. It’s likely that your pancreas is making enough extra insulin to keep your blood sugar levels out of the diabetic range, but eventually, it may not be able to make enough extra insulin. This means that blood sugar levels may continue to rise, along with your risk of developing diabetes.
Factors That Affect Your Blood Sugar
Food and Beverages
Carbohydrate-rich foods, such as fruit, starches, dairy, and concentrated sweets, can all cause a rise in your blood sugar, as can sugar-sweetened beverages like juice and soda. Alcohol, however, may lower your blood sugar, because alcohol disrupts the liver’s ability to produce glucose.
Stress
Stress can spike your blood sugar! When you’re stressed, your body releases hormones like adrenaline and cortisol. These hormones make it harder for insulin to properly do its job, which can cause blood sugar levels to rise. Over time, chronic stress may lead to insulin-resistance, which puts you at an increased risk of developing diabetes. This is why it can be so vital to focus on stress management tools with your Culina Health Registered Dietitian.
Dehydration
When you’re dehydrated, there is less water in your bloodstream, which makes everything else in your bloodstream more potent—including glucose! For this reason, dehydration makes you more susceptible to elevated blood sugar levels.
Hormonal Changes
In addition to stress, other types of hormonal shifts, such as the menstrual cycle (which can lead to fluctuations in blood sugar levels), menopause (which may make you more prone to low blood sugar), and birth control can all impact blood sugar levels.
Exercise
Exercise can either lower, or increase, your blood sugar—depending on the type of workout and the duration of activity. Things like heavy lifting, sprints, and competitive sports can all raise blood sugar, because they release stress hormones. A more low-impact workout, like yoga, walking or stretching, is more likely to decrease blood sugar.
Medication
Taking certain medications such as steroids, statins, beta blockers, antibiotics and decongestants may raise your blood sugar levels.
RD Strategies for Blood Sugar Balance
What to prioritize for blood sugar management
- Fiber
- Protein
- Sleep (7-8 hours)
- Hydration ( aim to drink half your body weight in ounces per day)
- Stress management
- Movement (aim for ~150 minutes of physical activity per week)
What to avoid for blood sugar management
- Sugar-sweetened beverages
- Alcohol
- Concentrated sweets
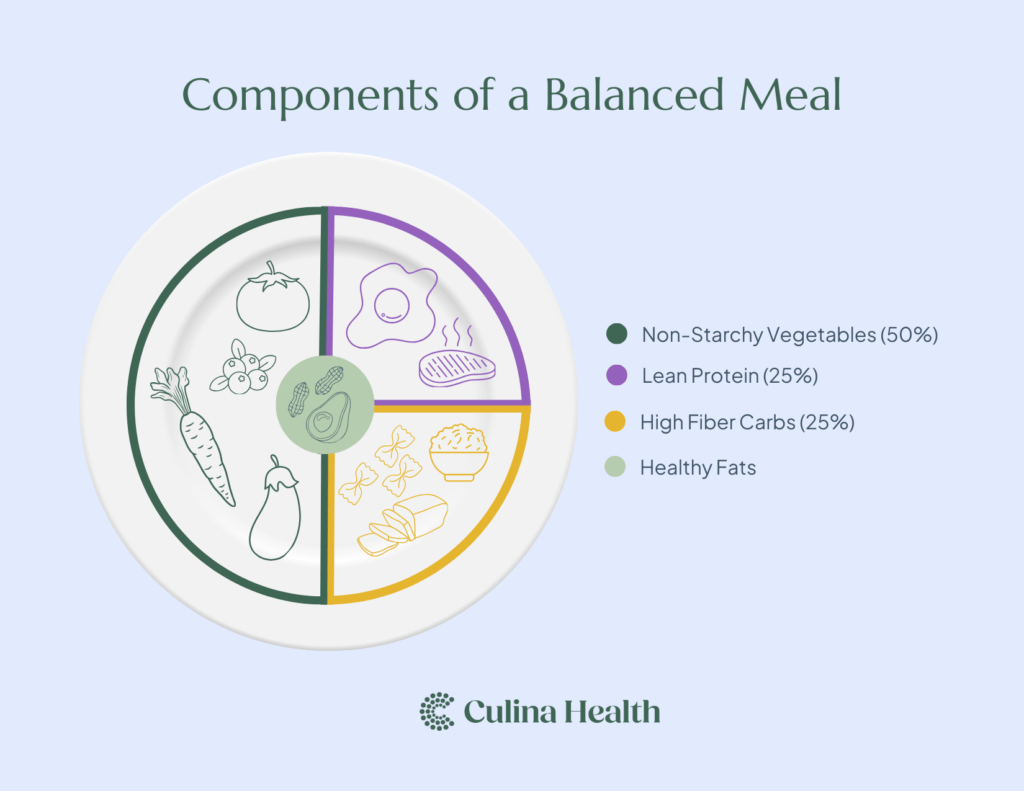
Components of a Balanced Meal
Balancing your meals is key to blood sugar stability. Combining your carbs with other nutrients helps support optimal blood sugar control. Components of a balanced meal/plate include:
Lean Protein (25%)
One-quarter of your plate should be lean protein. Great sources of lean protein include tuna, salmon, cod, skinless chicken, skinless turkey, sardines, clams, mussels, beans, lentils, tofu, tempeh, and edamame.
High-Fiber Carbohydrate (25%)
One-quarter of your plate should be carbs, but not just any carbs—high-fiber carbohydrates. Examples include whole wheat bread, whole wheat pasta, barley, bulgur, buckwheat, quinoa, wild rice, sweet potatoes, corn, butternut squash, and plantains.
Non-Starchy Vegetables (50%)
Half of your plate should be non-starchy veg. Think broccoli, cauliflower, zucchini, eggplant, kale, collard greens, cabbage, cucumbers, carrots, brussels sprouts, bok choy, and lettuces.
Building a Balanced Snack
To create a delicious snack that will support optimal blood sugar control, follow the recipe of high-fiber carb + protein or fat.
Blood sugar balancing snack ideas
- 1 medium apple with 1 tablespoon peanut butter
- ½ cup berries with 6-oz low-fat Greek yogurt
- 1 small banana with 1-2 hard-boiled eggs
- 1 slice whole grain bread with ¼ avocado
- 2 cups of popcorn with 1 low-fat string cheese
- 10-12 whole grain crackers with 2 tbsp. hummus & veggies
Get Personalized Support from a Registered Dietitian
If you want to go deeper on how to make the science of blood sugar balance work for your individual needs, get support from a Culina Health Registered Dietitian! Culina Health RDs can work with you to create personalized nutrition goals, adopt healthy habits around sleep, exercise, and stress management, and even troubleshoot any barriers or challenges to healthy habits that come up during the process. We can even work with your primary care provider to analyze and plan around your labs, symptoms, and diagnoses. Whatever you’re dealing with, our team is here for you, and we are in network with most major insurance plans! You can match with a Registered Dietitian today to get started on your health goals.





